Pemi-Baker Hospice & Home Health Supports Heart Health Month with Palliative Care for Heart Failure Patients
As February marks National Heart Health Month, Pemi-Baker Hospice & Home Health is proud to highlight its palliative care services tailored to support individuals living with heart failure. Heart failure is a challenging condition that profoundly affects the quality of life for patients and their families. With our specialized palliative care, individuals can find relief from symptoms and improve their overall well-being. 
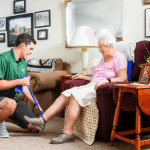
Living with heart failure can be an uphill battle, often characterized by breathlessness, anxiety, fatigue, and discomfort due to swelling in the extremities. These symptoms can significantly limit one’s ability to engage in daily activities and diminish the enjoyment of life’s pleasures. Recognizing these challenges, our palliative care team steps in to provide comprehensive support and alleviate distress.
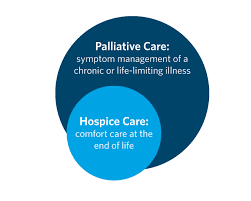
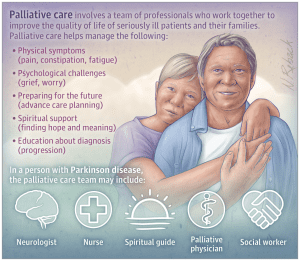
Palliative care, pronounced “pal-lee-uh-tiv,” is a specialized form of medical care designed to address the symptoms and stresses associated with serious illnesses such as heart failure. Our multidisciplinary team of doctors, nurses, and specialists collaborates closely with patients’ existing healthcare providers to offer an additional layer of support. Regardless of age or stage of illness, palliative care focuses on improving the quality of life for both patients and their families.
Heart failure presents a range of unpredictable symptoms, from fluid retention and breathing difficulties to pain and anxiety. Our expert palliative care team is adept at managing these symptoms and helping patients navigate the challenges they face on a day-to-day basis. Whether it’s providing strategies to improve breathing or offering techniques to reduce anxiety, our team is dedicated to empowering patients with the tools they need to cope effectively.
Beyond symptom management, our palliative care professionals serve as guides, assisting patients and their loved ones in navigating the complexities of the healthcare system. From facilitating discussions about treatment options to ensuring effective communication among healthcare providers, we strive to help patients make informed decisions about their care.
As we observe National Heart Health Month, Pemi-Baker Hospice & Home Health reaffirms its commitment to providing compassionate palliative care for individuals living with heart failure. Through our tailored services, we aim to alleviate suffering, enhance comfort, and promote dignity for patients and their families throughout their journey.
For more information about our palliative care services for heart failure patients, please visit www.pbhha.org or contact 603-536-2232.









 Your palliative care team can help you with all this and more. The team will be your sounding board and your first line of defense against any symptoms of pain, discomfort, depression or anxiety.
Your palliative care team can help you with all this and more. The team will be your sounding board and your first line of defense against any symptoms of pain, discomfort, depression or anxiety.