Pemi-Baker Hospice & Home Health Highlights Support for Cervical Cancer Awareness Month.
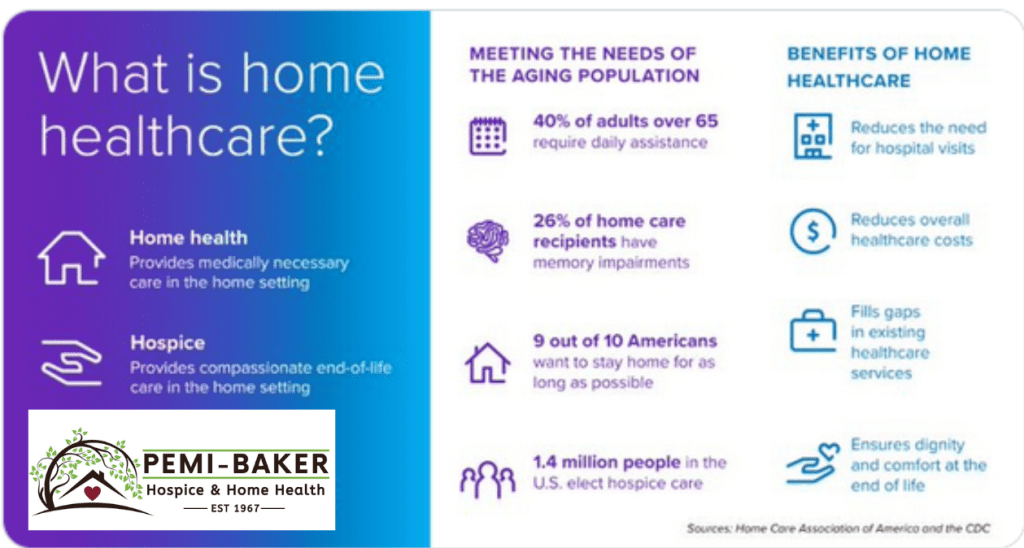
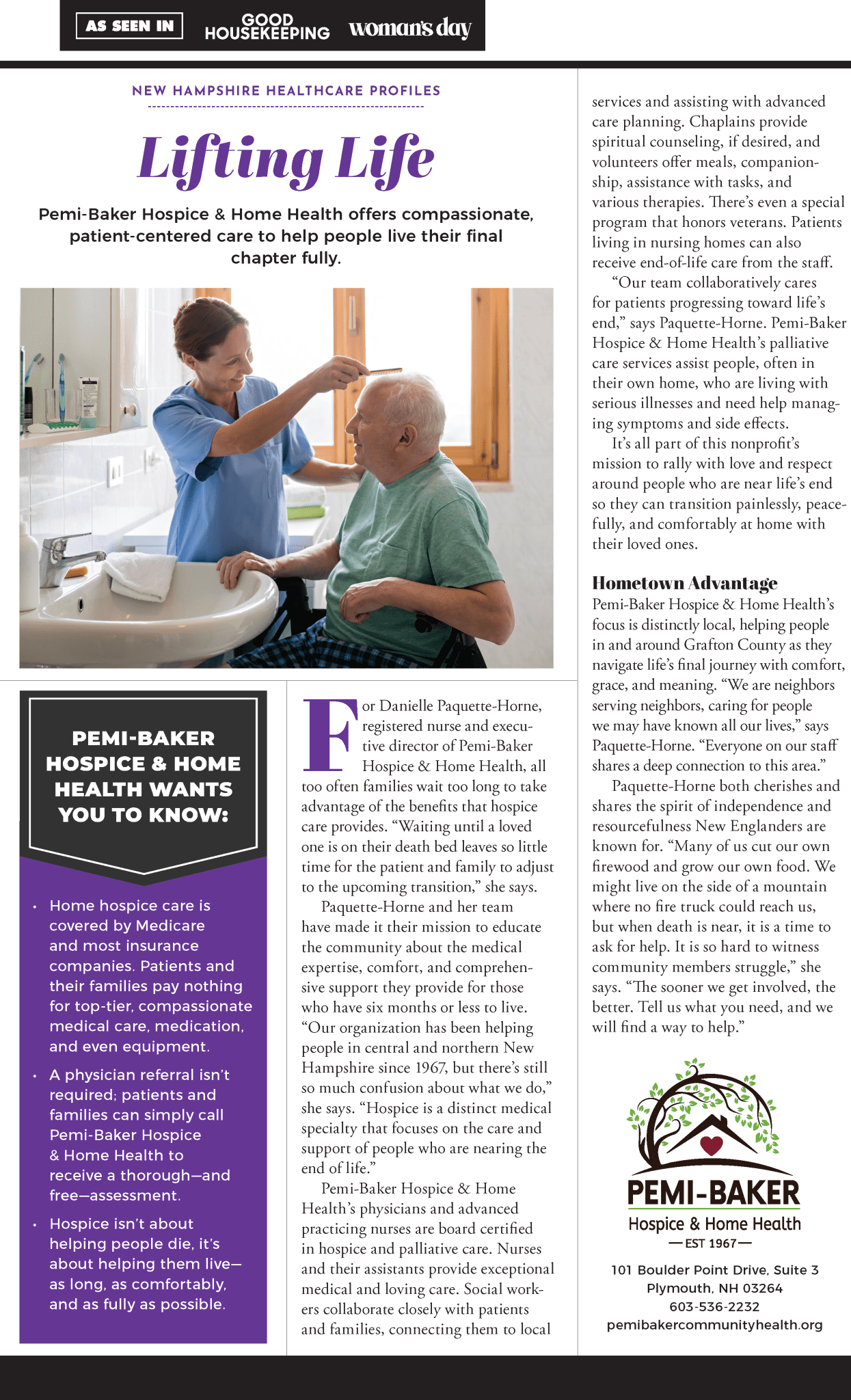
In recognition of Cervical Cancer Awareness Month, Pemi-Baker Hospice & Home Health emphasizes the importance of compassionate care for those living with cervical cancer. Through our Home Health team, we offer specialized palliative care to help patients find relief from symptoms, manage emotions, coordinate care, and navigate complex decisions. For those at the end of life, our hospice care provides a peaceful, supportive environment for patients and families.
Palliative care focuses on relieving the symptoms and stress of serious illnesses, improving the quality of life for both patients and their families. This care is provided by a dedicated team of doctors, nurses, and other professionals who collaborate with your existing healthcare providers. Whether you are undergoing treatment or managing long-term effects, palliative care can offer a crucial layer of support tailored to your needs.
“Hearing a diagnosis of cervical cancer can feel overwhelming,” said Aubrey Engle, RN, Executive Director, at Pemi-Baker Hospice & Home Health. “Our Home Health team is here to help you and your family find comfort and clarity, addressing physical symptoms, emotional well-being, and practical needs.”
When to Consider Home Health Palliative Care or Hospice
Palliative care through Pemi-Baker’s Home Health team is appropriate at any age and any stage of cervical cancer. Whether you are newly diagnosed, in the middle of treatment, or living with long-term side effects, this specialized care focuses on improving your comfort and well-being.
Services provided by our team include:
- Relief from physical symptoms like pain, nausea, and fatigue.
- Emotional and psychological support to address stress, anxiety, and depression.
- Assistance in understanding treatment options and making informed decisions.
- Seamless coordination between healthcare providers for comprehensive care.
For those reaching the final stages of their journey, Pemi-Baker Hospice & Home Health also offers hospice care, focusing on ensuring comfort, dignity, and peace for patients and their families. Our hospice care team provides compassionate end-of-life care, supporting loved ones every step of the way.
How to Access Care
If you or a loved one are living with cervical cancer, talk to your doctor about a referral to palliative care through Pemi-Baker Hospice & Home Health. “Our team works hand-in-hand with your primary healthcare providers to deliver personalized care plans,” said Engle. “Palliative and hospice care ensure you feel supported and empowered, no matter where you are in your journey.”
If you or a loved one are living with cervical cancer, ask your doctor about a referral to home health or hospice care. To qualify for home health care, a person must have a physician’s order and demonstrate a need for skilled care that can be safely provided at home. Our focus is on providing comfort to patients and support to families, with our team available 24/7 to address any concerns. The call is free, and our professionals are ready to assist you! Call us today at 603-536-2232 to learn more.








 Remember to think “FAST” and look for the following signs:
Remember to think “FAST” and look for the following signs: