Aquatic Physical Therapy is physical therapy that takes place in a pool under the supervision of a trained healthcare professional. Aquatic Physical Therapy is also known as aquatic therapy, water therapy, aquatic rehabilitation, aqua therapy, pool therapy, or hydrotherapy. Aquatic therapy continues to grow in popularity as a safe complement or alternative to traditional land-based therapy and it is suitable for children and adults of all ages and fitness levels. You do not need any swimming experience to gain benefits of the water.
Water therapy has been used for thousands of years throughout the world. Consider the following examples:
- Ancient Greeks and Romans bathed in hot springs to improve circulation and promote relaxation.
- Hippocrates recommended bathing in spring water as a way to treat sickness.

- Swiss monks were known to use thermal waters to treat sick or disabled people in their community.
- Japanese hot springs, or onsens, are said to have medicinal effects that include healing chronic pain, treating skin problems, and relieving constipation.
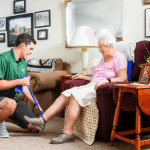
“The biggest benefit of aquatic therapy is that people who are injured, disabled or otherwise not capable of comfortably or safely performing exercises on land can easily do so in the water,” said Kaity Schwartzer, PT, DPT for Pemi-Baker Community Health. The natural buoyancy of water reduces stress on the body and helps patients exercise easier with less pain. Plus the natural pressure of water in therapy pools reduces joint and soft-tissue swelling and provides enough resistance to strengthen muscle.
Compared to other forms of physical therapy, aquatic therapy results in a higher client compliance rate and less pain throughout the recovery process. “Any opportunity to significantly minimize the pain a client experiences should be taken seriously because with less pain, a client can enjoy a higher quality of life,” said Schwartzer.
Another important advantage of aquatic therapy is that it can often begin before land-based therapy. For athletes looking to get back into competition, or busy professionals who want to recover from surgery as quickly as possible, this makes a water-based program the natural choice.
Pemi-Baker Community Health’s specialty-trained aquatic therapists will help you reach your goals. They provide safe, hands-on effective, customized care for patients with any of the following:
- Difficulty walking or limited weight-bearing capacity
- Fibromyalgia, Bursitis, Tendonitis
- Extremity injuries which prevent regular conditioning on normal surfaces or in athletic participation
- Spinal cord injury, Scoliosis, lower back pain
- Arthritis, Osteoarthritis, Rheumatoid arthritis
- Total hip/knee/shoulder joint replacements or reconstruction recovery
- Pregnancy-related musculoskeletal pain
- Cerebral palsy, Parkinson’s disease, Multiple sclerosis, Stroke, Traumatic Brain Injury
Aquatic therapy is different from aquatic exercise because it is a physical medicine and rehabilitation specialty that requires the involvement of a trained professional. Aquatic Therapy is covered by most insurance providers and you do not have to know how to swim. Common goals of aqua therapy programs include improving flexibility, balance and coordination, building muscle strength and endurance, enhancing aerobic capacity, assisting with gait and locomotion and reducing stress w hile promoting relaxation.
hile promoting relaxation.
PBCH’s licensed therapists will meet one on one with you, orienting you to the pool and changing rooms and assisting you around the perimeter of the therapy pool. COVID-19, CDC guidelines are strictly followed with clinicians and clients wearing masks and therapy sessions scheduled to prevent overlapping of clients in the locker rooms. We invite you to come by our facility to view the pool and get a tour!
~Anna Swanson



 comfortable at the end of their lives. Fewer people have heard of palliative care, and they may have no idea what it is. The truth is that
comfortable at the end of their lives. Fewer people have heard of palliative care, and they may have no idea what it is. The truth is that  often, board-certified in Hospice and Palliative Medicine. Additionally, the team generally includes a palliative care nurse, a social worker, a chaplain or someone who can help with spiritual support if the patient requests it, plus a patient navigator or someone who can coordinate the process. PBCH and NANA work collaboratively with
often, board-certified in Hospice and Palliative Medicine. Additionally, the team generally includes a palliative care nurse, a social worker, a chaplain or someone who can help with spiritual support if the patient requests it, plus a patient navigator or someone who can coordinate the process. PBCH and NANA work collaboratively with