Pemi-Baker Community Health, Mid-State Health Center and Speare Memorial Hospital are collaborating to provide The Healthy Aging Series: Hard Topics Made Easy for Seniors and Those Who Care for Them. The virtual series will be a mix of videos and podcasts designed to educate and assist seniors, caregivers, and the community about topics related to healthy aging.
Pemi-Baker Community Health, Mid-State Health Center and Speare Memorial Hospital are collaborating to provide The Healthy Aging Series: Hard Topics Made Easy for Seniors and Those Who Care for Them. The virtual series will be a mix of videos and podcasts designed to educate and assist seniors, caregivers, and the community about topics related to healthy aging.
Each month a new presentation will be available from an expert at Speare, Mid-State, or Pemi-Baker. The series launches July 1st with the first episode covering The COVID-19 Vaccine, presented by Mid-State Health Center’s Dr. David Fagan.
Future episodes will cover topics such as Home Funerals and Green Burials, Staying Fit Indoors and Out, Communicating with Your Aging Parent, Advanced Directives and more.
For a complete schedule of events, to learn more about the series, and to subscribe to episode notifications, visit www.virtualhealthseries.com.


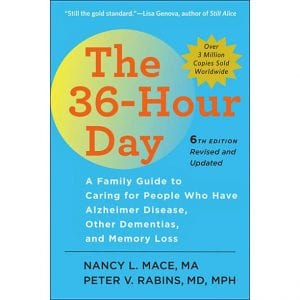 The book is THE 36-HOUR DAY: A Family Guide to Caring for People Who Have Alzheimer Disease, Other Dementias, and Memory Loss. The title itself, as does the book, pulls no punches. Providing ongoing care for a person with dementia is time-consuming, emotionally demanding, stressful, and exhausting, so that one’s days feel like they are longer than they are and packed with too much to do and remember.
The book is THE 36-HOUR DAY: A Family Guide to Caring for People Who Have Alzheimer Disease, Other Dementias, and Memory Loss. The title itself, as does the book, pulls no punches. Providing ongoing care for a person with dementia is time-consuming, emotionally demanding, stressful, and exhausting, so that one’s days feel like they are longer than they are and packed with too much to do and remember.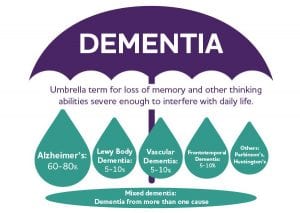 In this introductory section, there is a brief presentation raising the question “What Is Dementia?” The book is careful to explore all sides of the challenges of caring for someone with dementia. The authors really walk alongside the readers/caregivers in taking the first steps toward assuming the responsibility of caregiving. Having read the book, I am hard-pressed to discover any stone that has been left unturned. Let me be quick to say that not all dementia patients end up in nursing homes. Caregiving story endings vary from case to case, very much the result of the many factors both patients and caregivers bring to their own unique circumstances.
In this introductory section, there is a brief presentation raising the question “What Is Dementia?” The book is careful to explore all sides of the challenges of caring for someone with dementia. The authors really walk alongside the readers/caregivers in taking the first steps toward assuming the responsibility of caregiving. Having read the book, I am hard-pressed to discover any stone that has been left unturned. Let me be quick to say that not all dementia patients end up in nursing homes. Caregiving story endings vary from case to case, very much the result of the many factors both patients and caregivers bring to their own unique circumstances.
 “Let Food Be Thy Medicine and Medicine Be Thy Food” – Hippocrates. Hippocrates of Kos was a Greek physician of the Age of Pericles, who is considered one of the most outstanding figures in the history of medicine. He is often referred to as the “Father of Medicine.”
“Let Food Be Thy Medicine and Medicine Be Thy Food” – Hippocrates. Hippocrates of Kos was a Greek physician of the Age of Pericles, who is considered one of the most outstanding figures in the history of medicine. He is often referred to as the “Father of Medicine.”

 Starting at the wrist of one hand, let your thumb and fingers of the other hand softly massage the wrist, and then move across the back of the hand, and continue to gently massage each knuckle and joint of each finger. As you finish, use your fingertips to move in a circle in your palm. Then attend to the other hand. You may also want to lightly rub your palms together or even to softly clap your hands. To massage your head, gently let your fingertips move through your hair (or what you have left of it!). Do this a few times. Then gently tap your fingertips throughout and across your whole scalp, not forgetting the areas around your ears or at the base of your skull down to your neck. This also stimulates the movement of energy in our cranial area.
Starting at the wrist of one hand, let your thumb and fingers of the other hand softly massage the wrist, and then move across the back of the hand, and continue to gently massage each knuckle and joint of each finger. As you finish, use your fingertips to move in a circle in your palm. Then attend to the other hand. You may also want to lightly rub your palms together or even to softly clap your hands. To massage your head, gently let your fingertips move through your hair (or what you have left of it!). Do this a few times. Then gently tap your fingertips throughout and across your whole scalp, not forgetting the areas around your ears or at the base of your skull down to your neck. This also stimulates the movement of energy in our cranial area. For the purpose of focusing and directing your attention, only one is necessary. Use it as the daylight is ending. Simply direct your attention to the light, bringing to mind thoughts of past good times and the joy of affection shared with loved ones. The length of time you do this for does not matter too much, but respect the rhythm of your ability to concentrate easily. This isn’t supposed to be a chore or an assignment! It seems to be more profitable to do this in a quiet time without the distraction of other noise. This can be settling to the soul and bring your day to a peaceful end.
For the purpose of focusing and directing your attention, only one is necessary. Use it as the daylight is ending. Simply direct your attention to the light, bringing to mind thoughts of past good times and the joy of affection shared with loved ones. The length of time you do this for does not matter too much, but respect the rhythm of your ability to concentrate easily. This isn’t supposed to be a chore or an assignment! It seems to be more profitable to do this in a quiet time without the distraction of other noise. This can be settling to the soul and bring your day to a peaceful end.

 If a person is feeling tightness, pain, loss of range of motion or strength, or feel like their posture is being impaired, these can be signs identifying the need for physical therapy. Treatment for breast cancer is saving lives. Let us help you with these side effects of breast cancer treatment so you can regain your health in motion!
If a person is feeling tightness, pain, loss of range of motion or strength, or feel like their posture is being impaired, these can be signs identifying the need for physical therapy. Treatment for breast cancer is saving lives. Let us help you with these side effects of breast cancer treatment so you can regain your health in motion!
 condition is or how it manifests itself. The condition can occur when there is a loss of brain cells that produce a chemical called dopamine. The four common symptoms are: tremors, limb and trunk stiffness, the slowing down of movement and weak balance or coordination. About 500,000 people in the U.S. have Parkinson’s disease, with about 50,000 people being diagnosed each year, according to the National Institute of Neurological Disorders and Stroke.
condition is or how it manifests itself. The condition can occur when there is a loss of brain cells that produce a chemical called dopamine. The four common symptoms are: tremors, limb and trunk stiffness, the slowing down of movement and weak balance or coordination. About 500,000 people in the U.S. have Parkinson’s disease, with about 50,000 people being diagnosed each year, according to the National Institute of Neurological Disorders and Stroke. safer movements and improved quality of life.
safer movements and improved quality of life.
 use of adaptive equipment
use of adaptive equipment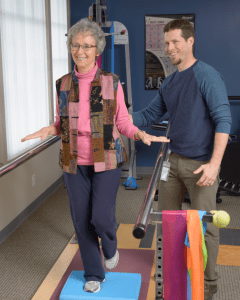 When you first meet your physical therapist, he or she will assess your balance. If it is impaired due to visual, inner ear or muscular reasons, your physical therapist will give you
When you first meet your physical therapist, he or she will assess your balance. If it is impaired due to visual, inner ear or muscular reasons, your physical therapist will give you Being part of a hospice team gives you the profound privilege of bringing comfort, peace and care to patients, caregivers, and their families during their transitional journey.
Being part of a hospice team gives you the profound privilege of bringing comfort, peace and care to patients, caregivers, and their families during their transitional journey.