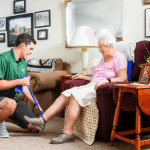
During the month of November, the home care and hospice community honor the millions of nurses, home care aides, therapists, and social workers who make a remarkable difference for the patients and families they serve. These heroic caregivers play a central role in our health care system and in homes across the nation. To recognize their efforts, we call upon all Americans to commemorate the power of caring, both at the home and in their local communities and ask them to join with Pemi-Baker Community Health in celebrating November as Home Care and Hospice Month.

In addition, Home Care Aide Week takes place the second full week of November. Join us in honoring these compassionate, tireless workers who play an invaluable role for their clients as caregivers, companions, and friends.
“Home care and hospice nurses, therapists, aides, and other providers choose to use their lives to serve our country’s aged, disabled, and dying. This noble work deserves our recognition and praise and we celebrate November as home care and hospice month for that very reason,” said National Association for Home Care & Hospice (NAHC) President William A. Dombi.
With 10 thousand Americans turning 65 every day, the need for health care will continue to rise, and costs will continue to skyrocket. This is where home care and hospice come in. As the preferred choice for most patients, it also offers the greatest cost savings. For example, Medicare pays nearly $2,000 per day for a typical hospital stay and $450 per day for a typical nursing home stay. Meanwhile, home care costs less than $100 a day and helps many U.S. seniors remain independent at home, enriching their lives, and staying in touch with those they love.
Fast Facts
- Home care providers will travel about 8 billion miles to deliver the best health care in the world.
- Ninety percent of Americans want to age in place, and home care is the preferred method of health care delivery among the disabled, elderly, and chronically ill.
- Home care provides high-quality, compassionate care to more than 5 million Americans annually.
With over 50 years of experience, serving clients from 22 towns in central and northern New Hampshire, Pemi-Baker Community Health is committed to creating healthier communities. Services include at-home healthcare (VNA), hospice and palliative care, on-site physical, occupational and aquatic therapy as well as free community educational/support groups via zoom.
~by Anna Swanson


 If a person is feeling tightness, pain, loss of range of motion or strength, or feel like their posture is being impaired, these can be signs identifying the need for physical therapy. Treatment for breast cancer is saving lives. Let us help you with these side effects of breast cancer treatment so you can regain your health in motion!
If a person is feeling tightness, pain, loss of range of motion or strength, or feel like their posture is being impaired, these can be signs identifying the need for physical therapy. Treatment for breast cancer is saving lives. Let us help you with these side effects of breast cancer treatment so you can regain your health in motion!
 condition is or how it manifests itself. The condition can occur when there is a loss of brain cells that produce a chemical called dopamine. The four common symptoms are: tremors, limb and trunk stiffness, the slowing down of movement and weak balance or coordination. About 500,000 people in the U.S. have Parkinson’s disease, with about 50,000 people being diagnosed each year, according to the National Institute of Neurological Disorders and Stroke.
condition is or how it manifests itself. The condition can occur when there is a loss of brain cells that produce a chemical called dopamine. The four common symptoms are: tremors, limb and trunk stiffness, the slowing down of movement and weak balance or coordination. About 500,000 people in the U.S. have Parkinson’s disease, with about 50,000 people being diagnosed each year, according to the National Institute of Neurological Disorders and Stroke. safer movements and improved quality of life.
safer movements and improved quality of life.
 use of adaptive equipment
use of adaptive equipment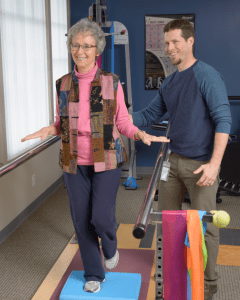 When you first meet your physical therapist, he or she will assess your balance. If it is impaired due to visual, inner ear or muscular reasons, your physical therapist will give you
When you first meet your physical therapist, he or she will assess your balance. If it is impaired due to visual, inner ear or muscular reasons, your physical therapist will give you Being part of a hospice team gives you the profound privilege of bringing comfort, peace and care to patients, caregivers, and their families during their transitional journey.
Being part of a hospice team gives you the profound privilege of bringing comfort, peace and care to patients, caregivers, and their families during their transitional journey.

 etcetera. With the ongoing pandemic, things aren’t that clean, direct, or explicit. The notion of a “new normal” brings with it the possibility that there may be some patterns of living we might not be able to recover. We are enduring a prolonged time of “not yet”. It is an experience of anticipatory grief on a global scale. It’s a hard place to be, and it may be awhile before we have any answers.
etcetera. With the ongoing pandemic, things aren’t that clean, direct, or explicit. The notion of a “new normal” brings with it the possibility that there may be some patterns of living we might not be able to recover. We are enduring a prolonged time of “not yet”. It is an experience of anticipatory grief on a global scale. It’s a hard place to be, and it may be awhile before we have any answers.

 hile promoting relaxation.
hile promoting relaxation. comfortable at the end of their lives. Fewer people have heard of palliative care, and they may have no idea what it is. The truth is that
comfortable at the end of their lives. Fewer people have heard of palliative care, and they may have no idea what it is. The truth is that  often, board-certified in Hospice and Palliative Medicine. Additionally, the team generally includes a palliative care nurse, a social worker, a chaplain or someone who can help with spiritual support if the patient requests it, plus a patient navigator or someone who can coordinate the process. PBCH and NANA work collaboratively with
often, board-certified in Hospice and Palliative Medicine. Additionally, the team generally includes a palliative care nurse, a social worker, a chaplain or someone who can help with spiritual support if the patient requests it, plus a patient navigator or someone who can coordinate the process. PBCH and NANA work collaboratively with